Myanmar – The Rose Clinic
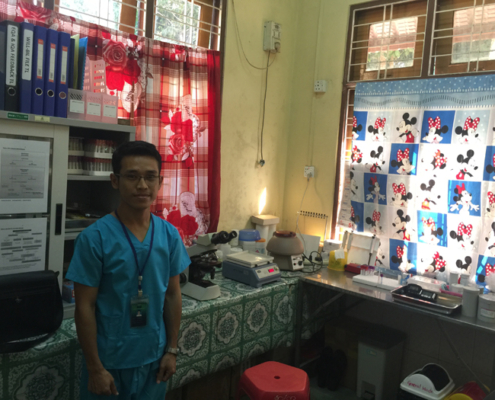
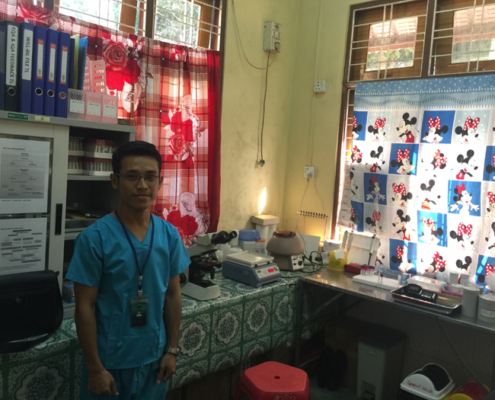
In 2013, FRS started a new project in Thanlyn, a poor, densely populated district, south-east of Yangon. We went in originally to improve the running of an existing free clinic which is next to the Free Funeral Services facilities. The clinic was under utilised as they rely on volunteer doctors with full time jobs elsewhere, and so can only serve a limited number of patients at early morning and lunch time. We went on to provide funding for the requisite medication and supplies; and for the needed team including 1 Medical Doctor, 1 project medical coordinator, 1 nurse, 1 lab technician, 1 outreach worker, 1 counsellor and one cleaner. This clinic has since grown substantially, currently operating 5 days a week, with 60-80 patients per day, or some 12,000 patient visits a year.
Interesting Fact : The local community is also very involved. There is now an ambulance service available for free and a new waiting area has been built. All these make the clinic cost effective and with good outreach to needy patients.
At FRS, we are pleased that the framework we provided (building of the Clinic, salaries for all the doctors, staff, general and medical supplies etc) had also facilitated the community to benefit in other ways – from food programmes, AIDs and TB medications.
Who We Work With:
We work with MAM (Medical Action Myanmar, managed by Dr. Frank Smithuis and Dr. Ni Ni Tun) which provides free medical treatment to the poorest in Myanmar.
Medical Action Myanmar (MAM) started its operations in June 2009 with the opening of a health clinic in Hlaingthayar Township, one of the biggest and poorest townships in Yangon. Since then, MAM activities have continued to expand with the opening of similar clinics in other areas of Yangon and the implementation of additional projects for the control of Malaria, Tuberculosis, HIV, malnutrition and basic health. In 2016, MAM has been running 4 clinics in Yangon (2 in Hlaingthayar, 1 in Shwe Pyi Thar and 1 in Thanlyn), 2 small clinics in the far north of the country (Putao, Kachin state) and 1 clinic in the Eastern region of Myanmar (Thanbyuzayat Township, Mon state). Meanwhile, MAM has developed a network of 1200 Community Health Workers (CHW) based in remote villages of Mon, Kayin, Thanintharyi, Kayah and Kachin states.
Interesting Facts :
MAM has a track record of very systematic data collection – these are very important in the fight against infectious diseases such as research into drug resistance in Malaria treatment and long term AIDS control. MAM has a very practical and effective approach to the management of healthcare for the localities of its operation.
Examples :
MAM clinics perform lab tests to investigate blood, stool, urine, spinal fluid, lymph node aspiration and skin smears. This is essential to come to a good diagnosis (including HIV, tuberculosis, malaria, syphilis (mother and child), anaemia, meningitis, penicilliosis, and cryptococcosis and so on. Despite the low budget and free consultations, test results are provided on the same day in order that the poor patients do not have to travel the long distances and incur the costs of a return journey. It even provides food for needy patients so they do not have to sell their medicine. They also provide simple food for relatives who come to the clinic to care for the severely ill patients on treatment days because such carers provide the emotional link with the patients, which is helpful. For needy TB patients, there are food packages provided by the World Food Programme consisting of fortified rice, cooking oil and other essentials.
(Check out MAM’s 2015 Annual Report with a heart-warming article on Dr. Ni Ni Tun and her incredible journey as healthcare provider).
Http://medicalactionmyanmar.com/data/bin/a57723d076b049_MAM_Activity%20Report_2015_FINAL.PDF
More about MAM
Clinics in Hlaingthayar, Yangon
Funds are mainly spent on direct health care, consisting of medicines, salaries of medical staff and for transport/freight/storage, water and sanitation and operational costs.
The most common pathology in children are respiratory tract infections, diarrhea and skin infections. All children who visit the clinic are also screened for malnutrition. Children with severe acute malnutrition (mortality of 50% if untreated), receive re-hydration and subsequently re-feeding with 6 meals a day in a step up schedule and treatment of underlying diseases (mostly TB or HIV) to reduce mortality to less than 10%. Besides the treatment, MAM also look into the social economic situation of the family in particular for orphans and children with single parents.
Family Planning
Many women have more children than they want and/or can care for adequately. This leads to poor health of both mothers and children. In addition, it leads to illegal abortion, which is usually performed in a non-sterile environment, leading to infection and death of the mother. This is mainly due to a lack of access or affordable family planning methods.
Aids prevention and treatment
In the Thazin clinic, comprehensive HIV care to families is given. This includes all aspects of HIV care, from testing and counselling to diagnosis and treatment of opportunistic infection, treatment with antiretroviral treatment and support for food and transport fees in case the patient has to visit regularly and cannot afford the charges. The aim is to have a one-stop service where all services are provided together in order to improve compliance and make it possible for the patient to live a normal life and return to their job and get income as soon as possible as opposed to many clinics where only a certain part of the services are provided and the patients have to be referred to other clinics for specific services.
HIV positive pregnant women form a specific group of patients – these women get preferential treatment. They are offered APT immediately to treat their HIV. This treatment not only saves their lives but also enables them to take care of their children, and is also highly effective to prevent HIV transmission to their unborn/born baby. The mothers are in the programme for up to 1.5 years after the birth of their baby.